.svg)
A Guide to CMS Dietary Regulations for Nursing Homes

Take Control of QA.
Make Inspections Effortless.

We’ll quickly uncover your needs and share how we can help—no pressure, no stress, just solutions. Grab your spot on our calendar today!
Be survey-ready every day with three simple dining audits

We’ll quickly uncover your needs and share how we can help—no pressure, no stress, just solutions. Grab your spot on our calendar today!
If you manage a nursing home, you are expected to serve food that is safe, well-planned, and matches each resident's personal preferences.
The Centers for Medicare and Medicaid Services (CMS) set strict dietary regulations for nursing homes. These rules explain what your food service must provide, how to plan menus, and how to accommodate dietary restrictions. They also cover staffing requirements, meal timing, and food safety.
This guide walks you through the CMS dietary regulations your nursing facility should follow. We'll also share some tips to help you meet these guidelines.
What Are CMS Dietary Regulations for Nursing Homes?
The CMS dietary regulations are the federal regulations you should follow if your nursing home is Medicare or Medicaid certified. These requirements are outlined in the State Operations Manual.
Under section 483.60, the CMS says that you should provide nursing home residents with a nourishing, palatable, and well-balanced diet. Meals should meet the resident's nutritional needs and match personal preferences where possible.
It's important to follow these rules to ensure quality care, reduce health risks, prevent malnutrition, and improve a resident's satisfaction.
Surveyors also use CMS rules during routine inspections. Your facility can receive citations if meals are missing, unsafe, or fail to meet the resident's dietary needs.
Plus, you won't be able to receive Medicare and Medicaid funding. This can affect operational viability and may lead to client loss.
Important CMS Guidelines for Food and Dietary Services
Food and nutrition service regulations are divided into several parts. Below, you’ll see what CMS expects for staff, menus, meals, special diets, meal timing, and food safety.
Staffing
You need food and nutrition services staff who will develop and oversee meal plans for residents.
To be specific, you should hire a qualified dietitian or other clinically qualified nutrition professional. Make sure this individual meets the following requirements:
- Holds a bachelor's degree or higher from a regionally accredited college or university in the United States (or an equivalent degree from another country) and has finished the academic requirements of a nutrition or dietetics program.
- Completed at least 900 hours of supervised dietetics work with a licensed dietitian or nutritionist.
- Has a license or certification as a nutritionist or dietitian in the state where the services are provided.
If a registered dietitian nutritionist is not employed full-time, you should assign a director of food and nutrition services. This person must be a certified dietary manager, a certified food service manager, or have a national certification for food service management and safety.
Besides dietitians or nutritionists, you need sufficient support personnel. They will safely fulfill the functions of the food and nutrition services. These do not refer to licensed nurses, nurse aides, or paid feeding assistants who assist residents with eating.
Menus and Nutritional Adequacy
The CMS mandates that menus should meet the nutritional needs of residents in line with established national guidelines and state requirements.
Prepare these menus ahead of time and follow them. Make sure they also reflect the religious, cultural, and ethnic needs of the resident population.
Your facility’s dietitian or other clinically qualified nutrition professional will review the dietary plans for nutritional adequacy.
It's important to serve food that is appetizing to and culturally appropriate for residents. This usually involves learning their needs and personal preferences.
Although individualized menus for all residents are not required, you should offer other options if they don't like the main choices. This ensures good health and satisfaction.
Food and Drink
Nursing homes should provide high-quality food and drinks to all residents.
Ensure that meals contain the highest possible nutritional value with a palatable, attractive appearance. This means avoiding the following:
- Prolonged food storage, light, and air exposure
- Holding food on steam tables
- Cooking in large volumes of water
You should also check if food is served at safe and appetizing temperatures to prevent scalds or burns.
Always consider a resident's allergies, intolerances, and personal preferences. Provide food substitutes that are consistent with the usual menu of your facility. For example, if the resident doesn't like grapefruit juice, you can offer another citrus juice or any vitamin C-rich juice that they will drink.
Lastly, serve drinks to ensure proper resident hydration. These include water and other beverages or food items that turn liquid at room temperature, such as popsicles and ice cream.
Therapeutic Diets
You can provide a therapeutic diet to treat a resident's medical condition, to decrease specific nutrients in their diet (e.g., sodium), or increase the nutritional intake of a certain mineral (e.g., potassium).
Your facility can also serve food that the resident is able to eat through a mechanically altered diet. This involves modifying the food’s texture to make it easier to chew and swallow.
However, you need to follow a strict diet ordered by an attending physician. This health professional should:
- Prescribe therapeutic diets
- Delegate to a qualified dietitian the task of prescribing a resident’s diet or a therapeutic diet to the extent allowed by state law
If the attending physician delegates this task, they should closely supervise the dietitian. They also remain responsible for the resident's overall health and well-being.
Meal Frequency
The CMS states that residents should receive three meals daily to significantly improve their quality of life.
This dietary regulation does not require a 24-hour full-service food operation or an on-site chef.
However, nursing homes must serve meals and snacks on a schedule that matches the resident's needs, preferences, and requests. For example, if they prefer to eat at non-traditional times, your facility should offer suitable and nourishing alternatives.
After identifying the resident's preferences and learning that it's outside the food service operator's working hours, your kitchen staff can prepare meals in advance. Then, the appropriately trained facility staff will serve food at non-traditional times.
The CMS also limits the time between supper and breakfast to no more than 14 hours, unless you provide a nourishing snack at bedtime and the resident agrees.
Food Safety Requirements
The CMS expects nursing homes to keep food safe, from delivery and storage to meal service. They recognize several food and beverage industry regulations, such as the U.S. Food and Drug Administration’s (FDA) Food Code and the Centers for Disease Control and Prevention’s (CDC) food safety guidance.
Your facility should follow these rules when procuring ingredients and raw materials. Choose sources that meet federal, state, or local standards.
It's also important to store and handle food with care to prevent the outbreak of foodborne illness.
Consider using a HACCP checklist to minimize food safety risks and meet regulatory compliance. Make sure to cover different factors that may contribute to foodborne outbreaks, such as:
- Unsafe food sources
- Poor personal hygiene
- Inadequate cooking temperature
- Contaminated kitchen equipment
How to Ensure Compliance with CMS Dietary Regulations?
Here are some tips to stay compliant with CMS dietary regulations for nursing homes.
Assess Residents’ Individual Needs and Preferences
Review each resident's nutritional status, current health conditions, swallow risk, and chewing ability.
You should also discuss their likes, dislikes, culture, and faith choices. Then, check if they need assistive devices when eating, such as special cups, plate guards, or spoons with foam padding.
These details help you learn what foods and textures are safe and helpful to each resident.
Develop Personalized Nutrition Care Plans
Use the assessment to create a diet plan that matches the resident's preferences, not just the diagnosis.
Include diet texture, liquid level, key food limits, and food goals in simple terms. Add preferred foods and backup choices.
Make sure to review the nutrition care plan during meetings. Seek feedback from a registered dietitian nutritionist or a director of food and nutrition services.
You should also involve the resident and their family in food choices.
When you notice that the resident's intake drops or their weight shifts, change the diet plan accordingly.
Train Staff on CMS F-Tags
F-tags are the labels that CMS surveyors use to record deficiencies during inspections. Each tag points to a specific rule, like menu planning, safe textures, or food temperatures. CMS uses F-tags to inspect every nursing home in the same way and ensure clear survey results.
Training staff on these tags is important to avoid citations and penalties.
To ensure proper staff training, you should pick a specific dietary regulation tied to an F-tag. Explain it in simple terms, then show what the rule looks like during meal prep and service.
You can also watch team members during meal prep times. Correct mistakes right away and teach them how to do it right next time.
Reward staff who perform consistently to improve motivation, performance, and knowledge retention.
Conduct Regular Food Safety Inspections
You should run food safety inspections on a set schedule.
Monitor meal temperatures at cooking, holding, and service, then record the results. Taste and look at food before it leaves the kitchen so you catch issues with flavor, texture, or appearance early.
Review tray accuracy during the tray line and again in the dining room, since wrong items or missing parts can put residents at risk.
You should also check staff hygiene, including hand washing, glove use, and clean uniforms.
Then, verify proper storage with clear dates, labels, and safe separation of raw and ready-to-eat food.
Don't forget to test equipment, like coolers, ovens, slicers, and dish machines, for correct function and clean surfaces.
Involve the whole nutrition services department in these audits, not just supervisors, to ensure consistency.
Consider using a food safety management audit checklist or an inspection platform like MyFieldAudits to simplify this task.
Review and Update Dietary Policies
Always keep your diet plans in line with current CMS regulations to match what they expect and avoid citations.
To do this, you first need to set a routine review, at least once a year or after any CMS update.
Compare your policies to the current CMS rules in food and nutrition services. Look specifically for gaps in menu planning, substitutions, therapeutic diet handling, meal help, and food safety logs.
Then, rewrite the steps of your plan using clear and simple language. Train staff on these changes right away to fit daily workflows.
Achieve CMS Regulatory Compliance With MyFieldAudits
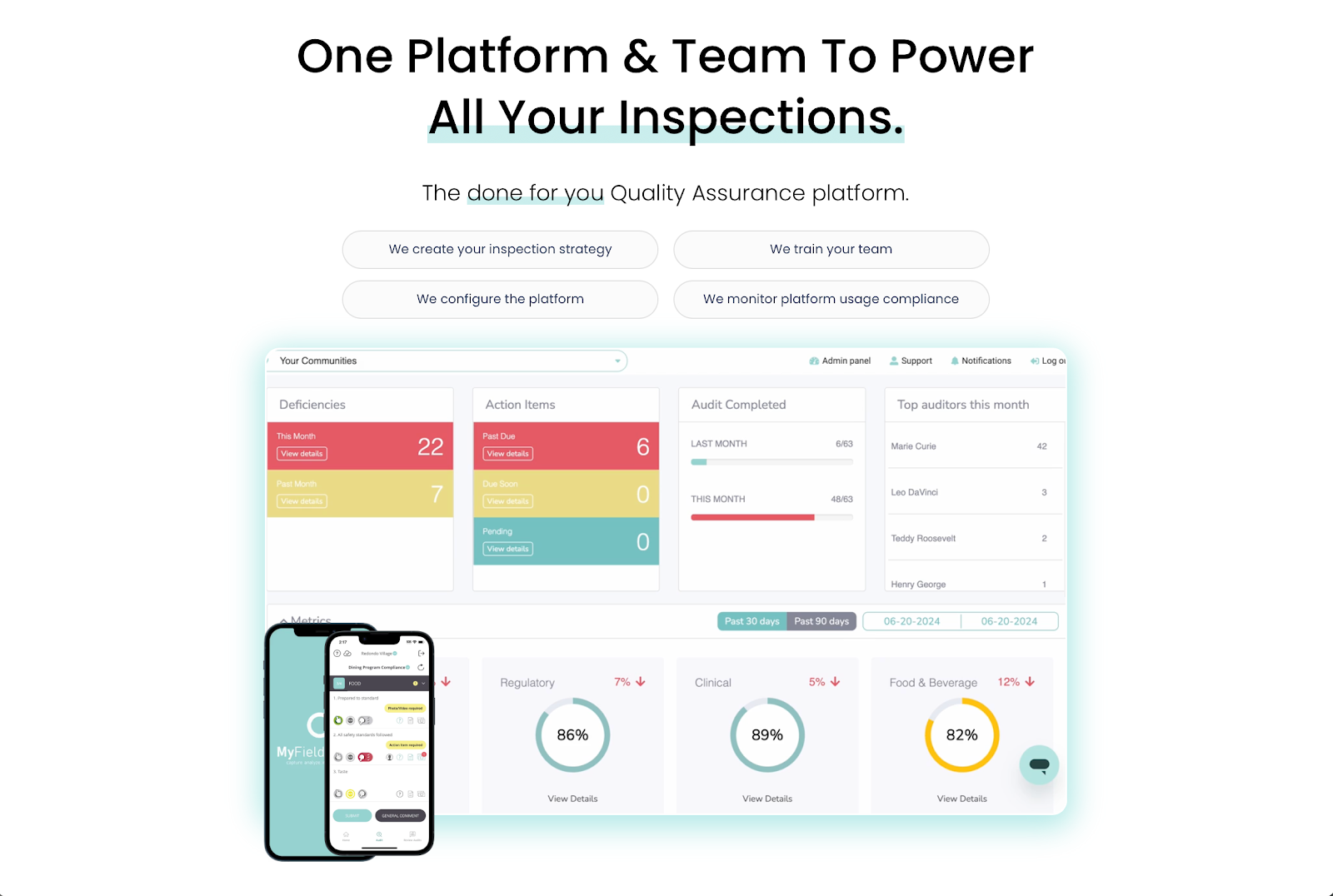
MyFieldAudits helps your nursing home meet CMS dietary regulations by making on-site checks simple, fast, and consistent.
Your kitchen staff can use the mobile inspection app to ensure tray accuracy, safe food temperatures, and staff hygiene in real time.
The platform automatically turns audit findings into clean, shareable reports that show proof of performance during CMS surveys. This also gives leadership teams and clients instant clarity on what’s really going on, which can build trust and retention.
However, MyFieldAudits is more than just another inspection software. It acts as your retention engine.
Industry experts will help you develop a strategy perfect for your facility's context, train your team, configure the platform, and monitor regulatory compliance. This helps you focus on providing a safe and excellent dining experience for your residents.
Schedule a demo today to keep quality assurance and compliance consistent through turnover! You can also check this product overview to see MyFieldAudits in action.
FAQs About CMS Dietary Regulations for Nursing Homes
Which is not a CMS requirement for food served in nursing centers?
CMS does not require a single fixed menu for every resident. You are not told to serve the same food to all people or follow a “one-menu fits all” plan. Instead, CMS focuses on meeting each resident’s needs, safety limits, and food choices while still keeping meals balanced and safe.
What is the final rule in section 483.60, food and nutrition services?
Section 483.60 is the CMS rule that sets food and nutrition standards for nursing homes. It mandates nursing homes to provide meals and drinks that meet daily nutrition and hydration needs, follow special diet orders, respect resident choices, and keep food safe. Surveyors use this rule during checks.
What food can be served at a nursing home?
You can serve any food that is safe for the resident and matches their diet order and personal preferences. Follow proper dietary management practices, such as offering nourishing alternatives, considering a resident's allergies, and keeping meals appealing.
How many meals per day does CMS require long-term care facilities to serve residents?
CMS requires at least three meals each day. There should be no more than 14 hours between dinner and breakfast unless you add a bedtime snack and the resident agrees.
%201.svg)





%201%20(1).svg)