.svg)
Important CMS Food Service Regulations to Follow

Take Control of QA.
Make Inspections Effortless.

We’ll quickly uncover your needs and share how we can help—no pressure, no stress, just solutions. Grab your spot on our calendar today!
Be survey-ready every day with three simple dining audits

We’ll quickly uncover your needs and share how we can help—no pressure, no stress, just solutions. Grab your spot on our calendar today!
The Centers for Medicare and Medicaid Services (CMS) set strict food service regulations for healthcare facilities. These rules outline staffing requirements, nutritional adequacy, food safety, meal frequency, and more.
It's important to follow these protocols to avoid citations, non-compliance fines, or loss of Medicare and Medicaid payments.
This guide breaks down the most important CMS food service regulations. We'll also share the best practices to implement to ensure compliance.
TL;DR
- CMS food service regulations require facilities to serve a nourishing, palatable, well-balanced dish for all residents at least three times daily.
- Facilities should hire sufficient staff with the necessary training, follow diet orders, respect resident choices, provide assistive devices, and meet food safety standards.
- The State Operations Manual outlines CMS rules governing food and nutrition services, provides guidance, and lists F-tags that surveyors check for compliance.
- MyFieldAudits helps facilities conduct real-time inspections and meet CMS regulations by providing a mobile-friendly quality assurance platform and expert support.
What Are CMS Food Service Regulations?
CMS food service regulations are federal laws that govern food and nutrition services in Medicare- and Medicaid-certified facilities. These are written in the State Operations Manual under section 483.60.
They require facilities to serve nutritious, enjoyable-to-eat, and properly balanced meals. Every dish served should meet daily nutrition requirements and any special diet orders based on medical conditions.
It's also important to consider individual preferences and personal dietary choices to enhance resident satisfaction.
CMS regulations make sure facilities support resident nutrition while respecting each person’s right to choose what they eat.
Which Facilities Should Comply With the CMS State Operations Manual?
Here are the facilities required to follow CMS food service regulations stated in the State Operations Manual.
- Nursing homes: Nursing facility settings should follow CMS dietary regulations and food service rules when providing meals to residents.
- Home health agencies (HHAs): HHAs engaged in providing food or nutrition services as part of patient care must comply with CMS regulations.
- Hospitals: Those that accept Medicare or Medicaid funding should meet CMS food service standards during inpatient stays.
- Other Medicare- or Medicaid-certified providers: Inpatient rehabilitation centers and other specialty care facilities should follow CMS food service rules when meal services are part of care.
Key CMS Regulations for Food and Nutrition Services
CMS sets clear rules on how facilities should manage food and nutrition services. Let's break them down into distinct categories:
Staffing
The CMS requires facilities to have sufficient staff to handle food and nutrition services each day. Staff should have the necessary competencies and skills to plan meals, prepare food, serve dishes, and help residents who need support for eating.
Food and nutrition services staff include a registered dietitian or another clinically qualified nutrition professional. This individual must possess the following:
- A bachelor's degree (or higher) in a nutrition or dietetics program from a regionally accredited university or college in the United States (or an equivalent foreign degree)
- A minimum of 900 hours of supervised dietetics practice with oversight of a registered dietitian or nutrition professional
- Certification or licensure as a dietitian or nutritionist in the state where the services are performed
If you don't have dietitians hired for a full-time role, you should designate a director of food and nutrition services.
The individual must be a certified dietary manager or a food service manager and hold a food safety certification issued by a nationally recognized certifying organization. They should meet state requirements and consult regularly with a qualified dietitian.
The director should also complete a course in food safety management that includes topics on managing dietary operations, sanitation procedures, foodborne illness, and food purchasing or receiving.
Menus and Nutritional Adequacy
Facilities should plan menus that meet the daily nutritional needs of residents. These menus must be written in advance and follow established national standards.
Meals should also reflect the religious, cultural, and ethnic needs of the residents.
The facility's dietitian or another clinically qualified nutrition professional should regularly review food items for nutritional adequacy. They must also update menus periodically to make sure food meets the residents' changing nutritional needs and clinical conditions.
Plus, it's important to learn individual needs by gathering feedback from residents and resident groups.
This doesn't mean you need individualized menus for all patients. However, with your facility's reasonable efforts, you should create a menu that considers residents' preferences and feedback.
Food and Drink
Facilities should prepare food in ways that keep its nutritional status, taste, and appearance. They must avoid prolonged exposure to food storage, light, and air, in addition to cooking in large volumes of water.
Kitchen staff need to serve dishes at a safe and appetizing temperature to prevent burns. Each meal should also accommodate the resident's allergies, intolerances, and personal preferences.
If residents refuse to eat the initial meal prepared, provide alternative options with similar nutritive value.
To maintain resident hydration, facilities should serve drinks, such as water and other liquids, that align with the resident's needs.
Therapeutic Diets
The CMS requires facilities to provide therapeutic diets when ordered by an attending physician or a licensed dietitian to the extent allowed by state law.
Prepare and serve diets exactly as prescribed. The goal is to treat the resident's disease or clinical condition, eliminate specific nutrients in the diet (e.g., sodium), or increase specific nutrients in meals (e.g., potassium).
If the resident has difficulty chewing and swallowing, kitchen staff can modify the food's texture. Serving a mechanically altered diet is only allowed if it is part of the physician’s or a delegated registered or licensed dietitian's order.
Frequency of Meals
Facilities should make sure that residents receive at least three meals daily. They must serve dishes at regular times comparable to normal mealtimes.
There should never be more than 14 hours between a substantial evening meal and the next day's breakfast.
However, if facilities provide nourishing snacks at bedtime, the span can extend up to 16 hours if a resident group agrees to that schedule.
The CMS does not require full-service food operations or an on-site chef working 24 hours a day. However, it mandates facilities to serve nourishing meals to residents who prefer to eat at non-traditional times or outside of scheduled meal service times.
Assistive Devices
Facilities should provide assistive devices, such as special eating equipment and utensils, for residents who need them.
For example, use foam padding in silverware handles to improve grip. Alternatively, install plate guards or invest in specialized cups to help patients with impaired coordination or tremor.
Staff should also have the necessary training to assist residents in using these devices when eating or drinking.
Paid Feeding Assistants
The CMS allows facilities to use paid feeding assistants for residents without complicated feeding problems.
Paid feeding assistants should complete a state-approved training program. This requires at least eight hours of training on feeding techniques, hydration support, communication skills, infection control, resident rights, and safety procedures.
Feeding assistants should only help residents if they're supervised by a registered nurse (RN) or a licensed practical nurse (LPN). In case of an emergency, they must contact a supervising nurse for help.
Food Safety Requirements
To ensure food safety compliance, facilities should only purchase raw materials or ingredients from sources approved by federal, state, or local authorities. This includes procuring food items directly from local producers.
Facilities must also store, prepare, and serve dishes according to food and beverage industry regulations.
If receiving food brought in by families or visitors, staff need to store and handle it properly to prevent foodborne illnesses.
Best Practices for Staying Compliant With CMS Food Service Regulations
Below are some best practices your facility can implement to ensure CMS compliance:
- Develop food safety checklists: Use HACCP checklists to identify food hazards, prevent contamination, and track corrective actions during every shift.
- Standardize food service policies: Create clear, written policies for food preparation, meal times, diet orders, ingredient substitutions, kitchen sanitation, and staff roles. This makes sure food service operations remain consistent across all shifts and locations.
- Conduct regular inspections: Walk through your facility to identify gaps in cleanliness, food handling, documentation, and staff performance before surveyors find them.
- Address deficiencies immediately: Correct food service issues as soon as they are identified and document actions taken to show ongoing compliance during reviews and follow-up inspections.
- Provide ongoing training: Train dietary and nursing staff regularly on food handling, diet accuracy, and resident assistance to keep daily practices aligned with CMS regulations.
MyFieldAudits Helps You Meet CMS Food Service Regulations
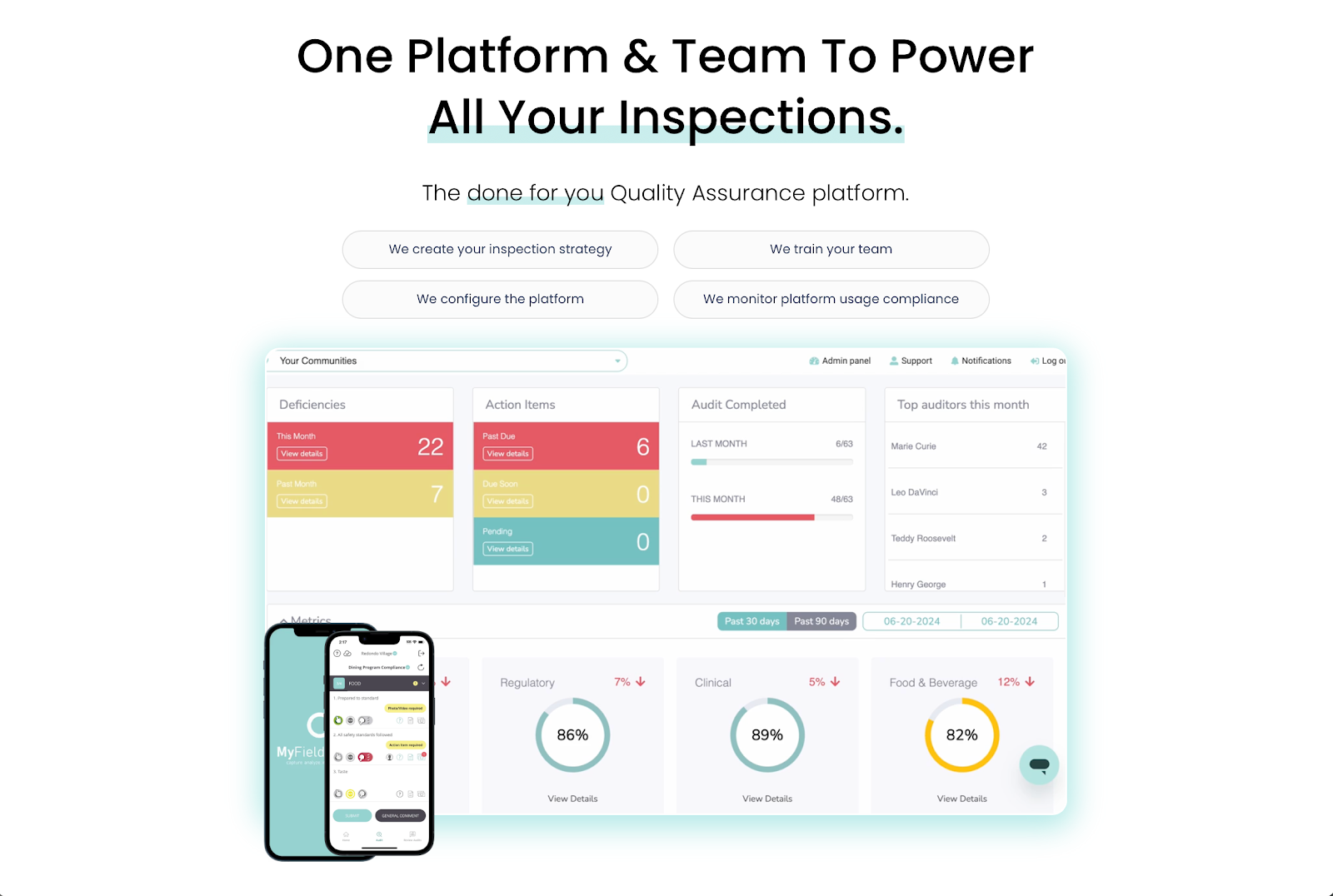
MyFieldAudits helps your facility comply with CMS food service regulations by giving you real-time visibility into daily operations.
Its mobile-friendly inspection platform lets you identify food safety hazards and fix on-site issues faster without lifting a spreadsheet.
Audit findings automatically sync to clean, shareable reports. These make it easier to show proof of performance to leadership teams and clients, which can build trust and retention.
However, MyFieldAudits is more than just another inspection software. It acts as your retention engine.
Industry experts will help develop an inspection strategy, deploy the inspection software, and monitor CMS compliance. This lets you spend more time delivering safe, high-quality meals to residents.
Schedule a demo today or watch this product overview to learn how MyFieldAudits handles the heavy lifting for your facility!
FAQs About CMS Food Service Regulations
What are the five guidelines for serving food?
The CMS expects food to be safe, properly prepared, served at suitable temperatures, matched to diet orders, and aligned with residents' choices. Facilities should also present meals in a form residents can eat, such as modified textures when ordered by an attending physician.
What is a CMS regulation?
A CMS regulation is a federal rule issued by the Centers for Medicare and Medicaid Services. These rules set standards that healthcare facilities should follow to take part in Medicare or Medicaid programs and are enforced during surveys.
Which is not a CMS requirement for food served in nursing centers?
The CMS does not require gourmet meals or restaurant-style service running 24 hours a day. The focus is on meeting nutritional needs, diet orders, safety rules, and resident preferences, not on offering luxury food options or specialty dining experiences.
%201.svg)





%201%20(1).svg)